Funding & Programming: Ending the HIV Epidemic Initiative (EHE)
BACKGROUND
Ending the HIV Epidemic in the U.S. (EHE), announced in 2019, aims to end the HIV epidemic in the United States by 2030. Agencies across the U.S. Department of Health and Human Services (HHS) developed an operational plan to achieve this goal, accompanied by a request for increased annual funding—including for AETC programs.
EHE leverages critical scientific advances in HIV prevention, diagnosis, treatment, and outbreak response. It focuses on 57 geographic areas where HIV transmission occurs most frequently, providing these jurisdictions with additional resources, expertise, and technology to support the development and implementation of locally tailored EHE plans. In the MAAETC region, the focus areas include Philadelphia, Baltimore, and Washington, D.C.
The initiative seeks to reduce new HIV infections by 75% by 2025 and by 90% by 2030—potentially averting an estimated 250,000 HIV infections.
EHE is structured around four key strategies: Diagnose, Treat, Prevent, and Respond.
MAAETC & EHE
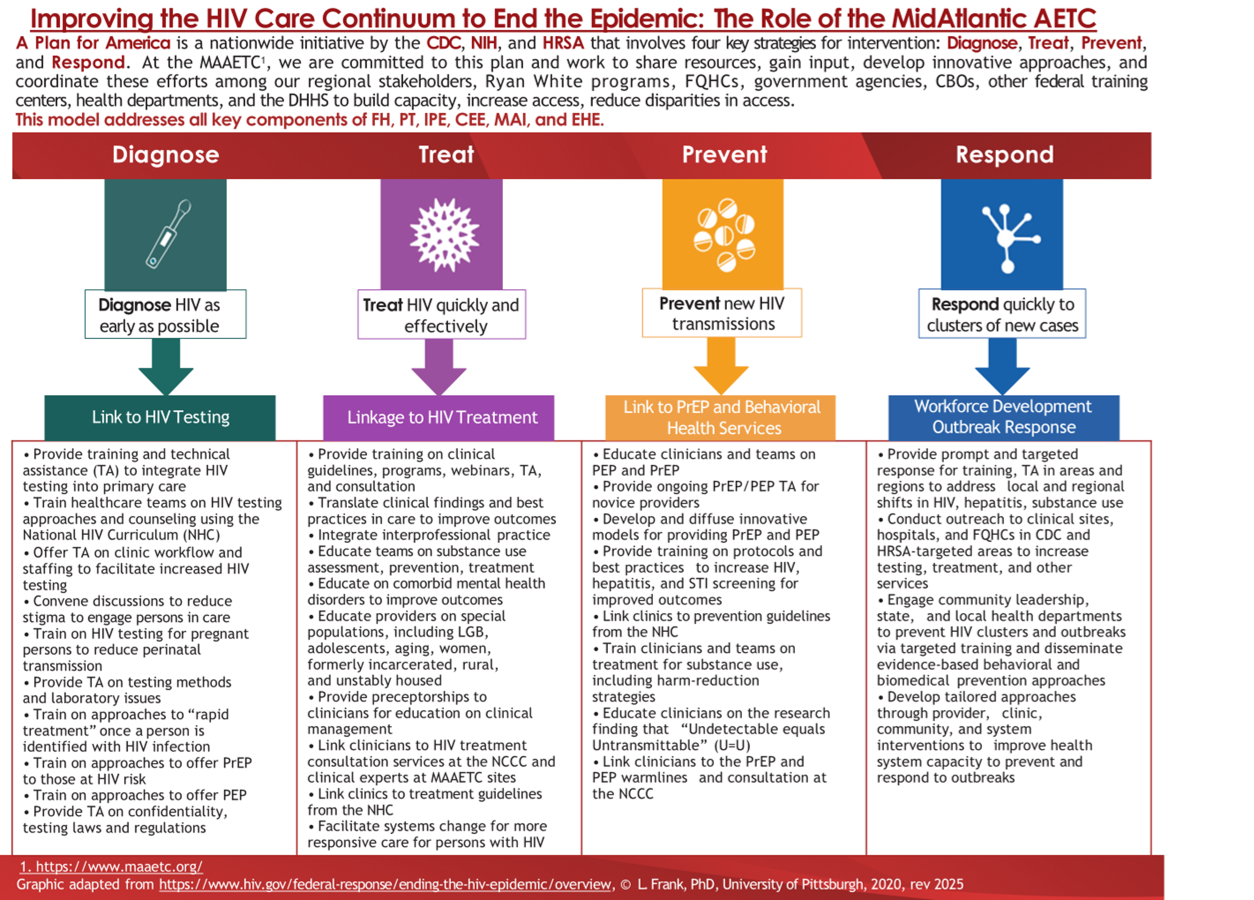 The MAAETC works with a broad range of partners across all sectors of society, including people with or at risk for HIV; city, county, and state health departments; local clinics and healthcare facilities; healthcare providers; providers of medication-assisted treatment for opioid use disorder; professional associations; advocates; community- and faith-based organizations; and academic and research institutions.
The MAAETC works with a broad range of partners across all sectors of society, including people with or at risk for HIV; city, county, and state health departments; local clinics and healthcare facilities; healthcare providers; providers of medication-assisted treatment for opioid use disorder; professional associations; advocates; community- and faith-based organizations; and academic and research institutions.
MAAETC supports the implementation of jurisdictional EHE plans and contributes to the planning, design, and delivery of HIV prevention and care services essential to the initiative’s success.
Local Partners (LPs) in Baltimore, Philadelphia, and Washington, D.C. maintain collaborative relationships with Ryan White Planning Groups, Ryan White Part A and B-funded providers, community health centers, and hospital emergency departments to identify and address gaps in HIV testing, treatment, and prevention services.
LPs conduct ongoing outreach to community health centers to assess their capacity to prescribe PrEP, support status-neutral HIV screening, and implement clear linkage-to-care protocols. Technical assistance and training are provided as needed.
In response to new HIV case clusters, LPs in EHE jurisdictions collaborate with local and state health departments to identify community training and TA needs.
LPs also ensure providers remain up to date when HHS updates HIV clinical guidelines for screening, prevention, and treatment. Updates are disseminated across the region, and LPs offer site-specific training and TA to primary care providers, community health centers, and experienced HIV clinicians.
In 2023, LPs responded to increased demand for training and TA related to newer injectable PrEP and HIV treatment options. They engage expert presenters to lead interactive trainings, case discussions, clinical preceptorships, and practical implementation sessions—translating updated clinical guidelines into actionable protocols for healthcare teams and patient education.



